Once I figure out how to, I would love to have the Hamilton song “The Room Where It Happens…” playing in the background while you read this. Alas, until I get techanically savvy, here is a YouTube Link and you can play it yourself…
“Talk less….” “(Smile) Listen more…”
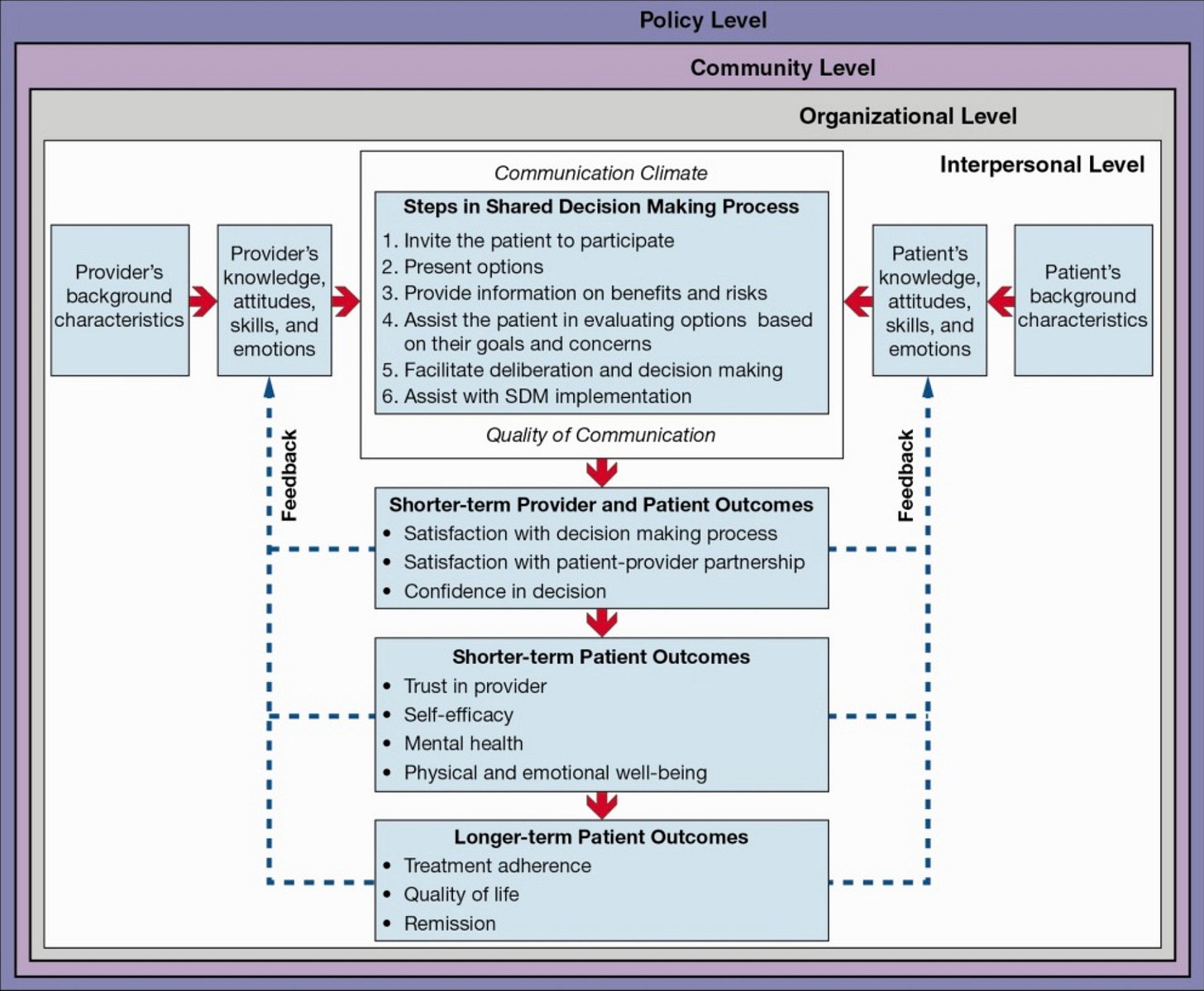
There are many models in the literature about “shared decision making,” and the one that resonates the most with me is from 2014 by Kane et al., as shown below. We will focus on the Interpersonal level of communication here.
This is a comprehensive model that evaluates all individuals in the room where the decisions are made. Working from the outside to in, our background characteristics, knowledge, attitudes, skills, and emotions can be defined as “patient worldview” and “physician worldview.” Later on, we will discuss physician worldview in detail as it is a very important and not well explored area of research and one of my colleagues, Login George PhD is focusing on it. Outcomes are an important part of SDM, and we will discuss those in a later post as well.
A brief moment on the patient worldview
In the SPIKES model, we assess patient perceptions by using open-ended and facilitating questions to listen to their story. We listen to what and how they represent their understanding of disease and how they speak about their hopes and worries. We listen to learn their language and framework to communicate more effectively.
The room where it happens…
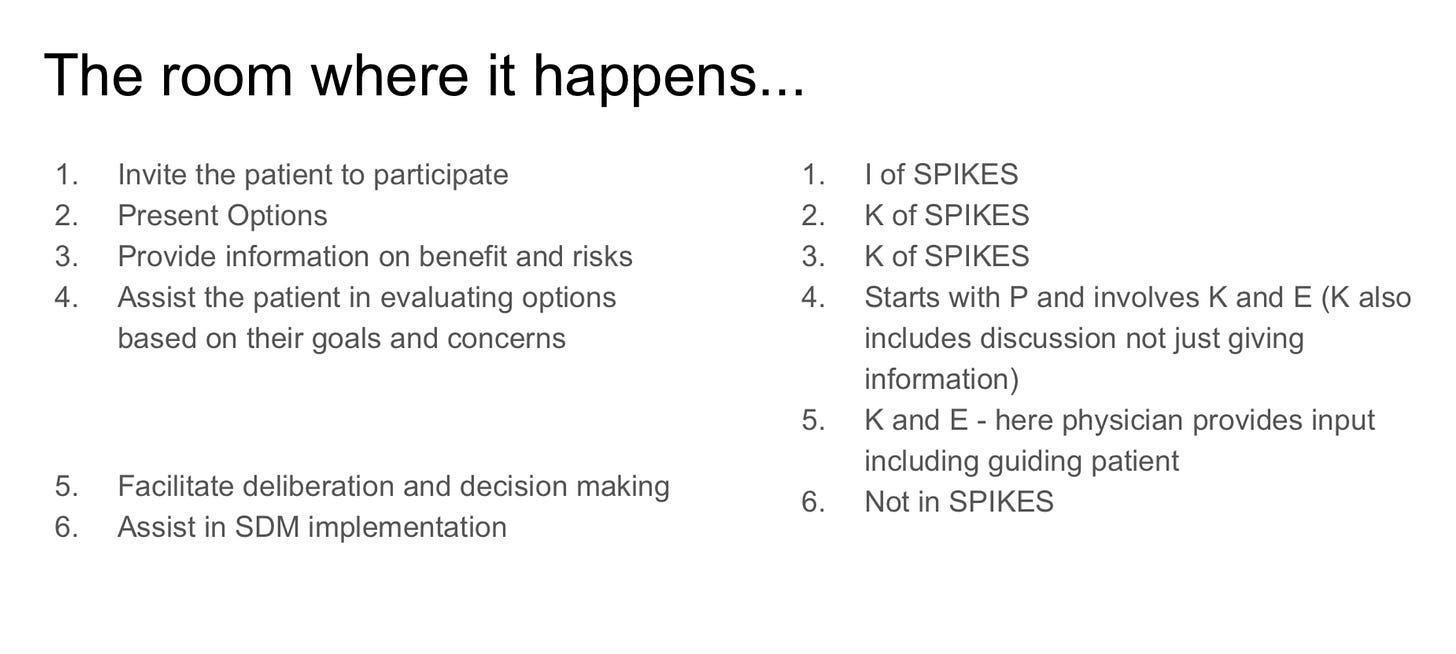
Steps in shared decision-making are easily translated into the SPIKES model. With one exception, implementation of the plan is not part of the SPIKES model.
Setting up the conversation and Assessing perceptions or the “SP” of SPIKES are done before we walk into the room and start the shared decision-making process. We can use the patient’s framework and language during this process to ensure we communicate clearly.
The first step in SDM is inviting patient to join the discussion. This is the same as invitation in SPIKES. A simple phrase such as “shall we discuss the next steps?” As an invitation to start listening to our input.
The second step is to present options, and depending on the situation, this could be broken into multiple steps. For example, if this is a cancer patient with numerous therapy choices, including clinical trials, having an overarching discussion of “we will discuss three options for therapy today.” Occasionally, I will ask the patient which order they want to hear the options. Other times, I will go with the standard-of-care and trial options, and rarely the other way around.
The goal is to ensure that the patient and family hear all the options, including the risks and benefits of each option. Providing any information, specifically, any information that is potentially negative, would require time to process and require empathic responses to ensure they actually hear what we say. So providing Knowledge goes along with Empathic responses to address emotions. Checking in with the patient after each option to ensure they have understood the risks and benefits before moving to the next option allows them to process information and help with the next step.
As all of the options are being discussed, patients may provide insights into their preferences. It is important for us to listen to their preferences and to ensure that they have heard all the options and weight the risks and benefits. CAVEAT: you will have your own opinions about what is the preferred option. It is, of course, your responsibility to provide your insights. It is important for physicians to provide their guidance and input while keeping patient’s preferences in mind. Occasionally, patients may prefer an option that is NOT your preferred option. You will likely question their choice, to ensure they understood the choices correctly. Though, you will likely not question when they agree with you. For optimal SDM, understanding how patient arrived at their prefered choice regardless of what they choose is advisable.
Be careful to avoid confirmation bias by only questioning when someone does not agree with you. Ensuring that they arrive at the right conclusion (therapy choice) requires us to question their understanding regardless.
This part of checking their understanding and rationale for their decision facilitates deliberation in decision-making.
Once a decision has been made with agreement from the patient and physician, it is time to implement the plan so that there is a maximum chance of success.
This post is the first of a series of posts that will focus on how SPIKES can be used with other models of communication for special uses. In future posts, we will cover, Serious Illness Conversation from Ariadne Labs; Motivational Interviewing; Ask-Tell-Ask and possibly other models. One of the most significant meta-cognitive messages from these posts is that while I learned and framed everything in the SPIKES model, someone else could easily write similar posts using a different acronym.
The overarching principle is that have a framework for communications and use it regularly to improve on your skills.
Thank you again for reading. Please share your thoughts and comments. Your engagement is key to my success.
Biren Saraiya MD


I hope that in the near future not only oncologists but physicians of all specialties will understand and get trained in this essential paradigm of shared decision making. Thank you for sharing your knowledge.